Yesterday, a tax-cut bill worth $4.5 trillion was approved by the Senate, with the final touches being added to its healthcare amendments as the Republican contingency attempted to rally their members. This legislation would institute the deepest reductions in federal healthcare expenditure ever, and denotes the most substantial transformation for the sector since the introduction of the Affordable Care Act in 2010.
The most recent draft of the bill presents some key alterations, including the exclusion of clauses that would have restricted federal funds from Medicaid and the Children’s Health Insurance Program being directed towards gender-affirming care. However, another clause that would cut off Planned Parenthood from Medicaid was preserved, a move that the organization insists could result in the loss of a quarter of the country’s abortion providers.
The following phase involves the House either approving the Senate’s draft of the bill or embarking on potentially protracted talks. President Trump aims to sign the bill by July 4 — just a couple of days from now. The trajectory for healthcare isn’t the only graph shifting as we approach 2023, trends in adolescent surgeries are also changing.
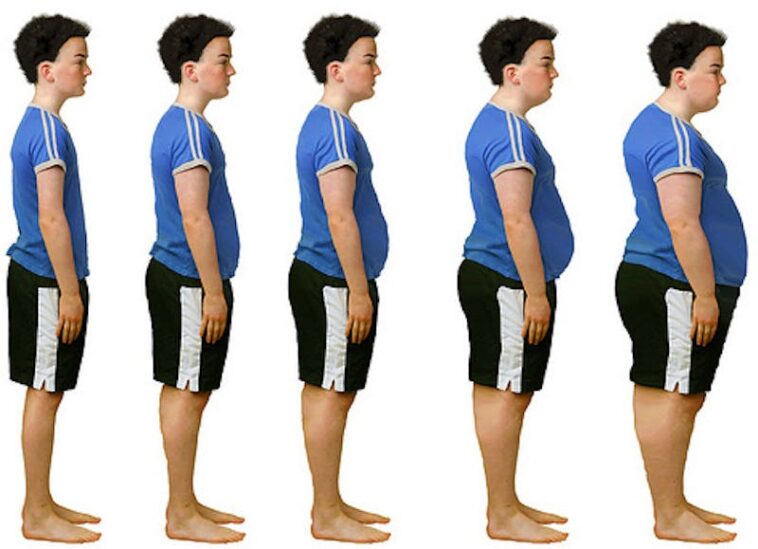
Between 2021 and 2023, the quantity of American teenagers undergoing metabolic and bariatric surgery surged by nearly 15%, as asserted by a study published in the current month’s edition of the Journal of Pediatrics. This trend persisted even after GLP-1 medications were given the FDA nod as a recognized obesity treatment for teenagers in December 2022, with the number of surgeries on the rise among teenagers in 2023.
In a departure from this trend, 2023 saw a decrease in the number of these surgeries performed on adults. Delving into the demographics further, the study highlighted that the uptick in these surgeries was prompted predominantly by Black and Hispanic adolescents. This signifies better access to, and acceptance of, a treatment considered the ‘gold standard’ according to the study’s authors.
It may, however, also denote unequal access to newer, less invasive GLP-1 treatment options. The CDC issued an MMWR report indicating that although Black teenagers have a 27% heightened rate of severe obesity compared to their white counterparts, in 2023, they were 39% less likely to receive a prescription for obesity medication.
The traditional consensus among researchers is that socioeconomic components play a key role in racial discrepancies observed in lung cancer rates. However, the specific impact of residential segregation has not been comprehensively examined. A research study published recently in JAMA Network Open suggests a potent relationship between a Black individual’s place of residence and their lung cancer risk.
The analysis evaluated a group of over 71,000 individuals residing in Southern states from 2002 to 2019. Lower levels of residential segregation were significantly linked with a decreased risk of lung cancer among Black participants — an association that was not observed in their white counterparts.
Some factors mediated this link. The study found both menthol smoking and exposure to fine atmospheric particulate matter played a role in almost half of the association between segregation and cancer. However, the authors stress that this still leaves more than half of the variance in lung cancer risk among Black individuals without a clear explanation.
While a considerable amount of work still needs to be conducted to alleviate segregation, the authors suggest that simultaneous public health efforts should be directed towards mitigating these intermediary factors. They emphasize the necessity of reviewing the impact of these mediating elements alongside broader social determinants in constructing comprehensive public health strategies.
The study serves as a call to policymakers to reassess the broader societal influences contributing to these health disparities. It underlines the importance of improving access to healthcare services, including emerging treatments and preventive strategies, particularly for underrepresented ethnic groups.
Moreover, the report underscores the importance of examining race-specific impacts when assessing population health trends and interventions. These findings can inform healthcare policies that better serve all demographics and work towards reducing health disparities.
In retrospect, with the tax-cut bill on one hand and the medical trends on the other, it is evident that legislative decisions can greatly affect community healthcare paradigms. This raises vital concerns pertaining to future healthcare reform, and asserts the need for policies that are considerate of racial and ethnic differences in healthcare access and outcomes.
On a grander scale, the responsibility of making healthcare more accessible and effective lies not just with healthcare professionals and policy makers, but also with society as a whole. It underpins the urgent need to challenge social norms, improve medical infrastructure, and advance public health education.